Setting the Record Straight
When the media sells us fiction, public debate pays the price. Here’s a recent Arkansas Business article, re-edited for TRUTH.

Partners for a Healthier Arkansas is bringing stakeholders together to encourage reforms that will help Arkansas’ Medicaid program better serve its beneficiaries and generate significant savings for taxpayers. We want to ensure the voices of all Arkansans’ are heard in developing solutions that puts the risk on managed care companies not taxpayers or beneficiaries. The result we are seeking is a system that is more accountable to the taxpayers, lowers costs and improves healthcare outcomes for patients.
Managed care, when extended to all populations, can save the state of Arkansas $2.5 billion over the next five years while providing the best service to Medicaid customers at the best price for taxpayers.
The Stephen Report
"Managed care provides a structure that allows a state Medicaid agency to establish specific quality benchmarks, to measure performance relative to those benchmarks, and to relate reimbursement to quality of care, quality improvement activities, and health care outcomes."
The Kaiser Commission of Medicaid and the Uninsured
Arkansas has overly high utilization of many high-cost services and has failed to implement best practices to effectively manage Medicaid costs.
The Stephen Report
39 states including Washington DC have implemented Medicaid managed care through risk-based, capitated Medicaid health plans.
The Kaiser Commission of Medicaid and the Uninsured
Managed Care organizations are supported by broad experience and industry tools. Utilizing financial metrics for tracking costs and measuring risks allow MCOs to maintain competitive MBR levels and encourage program stability.
When providers apply state-of-the-industry tools for measuring patient outcomes to Medicaid, Managed Care allows tracking of not only quantity but quality of care, as determined by the National Committee for Quality Assurance.
Managed Care moves Medicaid from a pay-per-claim model to one that pays for performance and better patient outcomes. Because MCOs assume the risks, it is possible to establish a fair, transparent and more predictable rate setting.
When the media sells us fiction, public debate pays the price. Here’s a recent Arkansas Business article, re-edited for TRUTH.
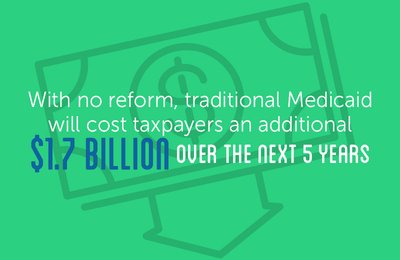
With no reform, traditional Medicaid will cost taxpayers an additional $1.7 billion over the next 5 years.

Proposed Bill of Rights Promises No Cuts To Reimbursement Rates. A proposed bill of rights supported by Governor Asa Hutchinson requires that all MCOs continue the exact same reimbursement rate as today to ...
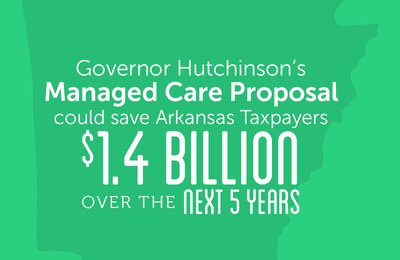
According to the Stephen Group, Governor Asa Hutchinson’s managed care plan for developmental disability and behavioral health populations would save $1.439 billion over five years. When ext ...
Arkansas has an opportunity to go from “lagging” to “leading” in Medicaid with a focus on quality of care, performance-based payments, and improved health care outcomes.
Arkansas can save $2.5 billion over the next five years while providing the best service for Medicaid customers at the best price for taxpayers.
Moving to Medicaid managed care will mean the availability of additional funding for other important priorities like schools, roads, and prisons.
Utilization of Managed Care for Medicaid participants and the projected $2.5 billion in savings is possible without expansion of the Private Option. These are separate programs.