The Managed Care Difference
The governor’s recent decision to delay the vote about Medicaid Managed Care has finally separated the discussion over Managed Care from the heated debate over “Arkansas Works,” formerly known as The Private Option. This division allows Medicaid reform proponents to educate the public about the benefits of a Managed Care system for certain high-cost groups of Medicaid recipients, specifically the developmentally and mentally disabled. Just to be clear, Managed Care is simply a method of structuring Medicaid in a way that provides a better quality of care for the money.
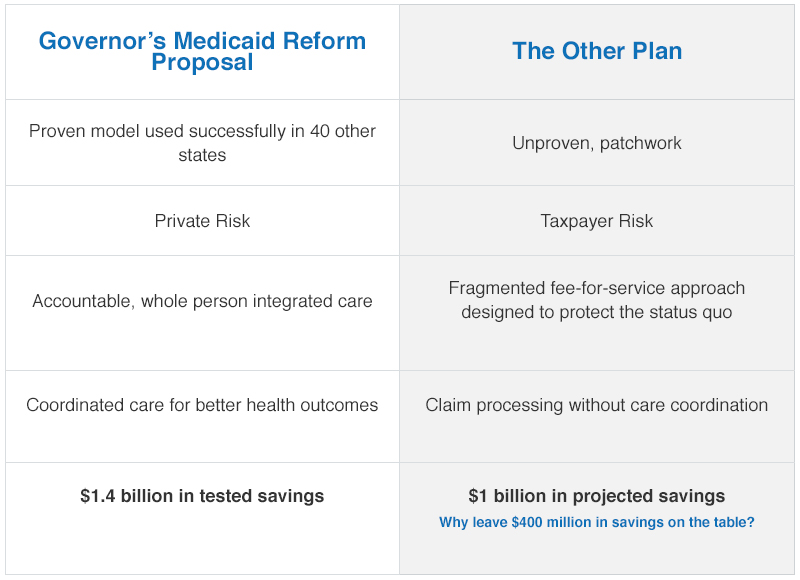
There are currently two plans vying to solve the Medicaid inefficiency problem. One of these plans is the governor’s Managed Care Proposal; the other is a patchwork approach known as Diamond Care.
Let’s consider each.
Medicaid Managed Care is a proven model that is used successfully in various ways in 40 other states and has resulted in improved health outcomes. Unlike Arkansas’ current fee-for-service model, Managed Care is a whole person-centered approach to health care. For instance, the plan will not only make certain that participants are connected to primary care physicians, but will also make sure they have necessary transportation, and that they take their medicine and attend follow-up visits.
The Managed Care model is administered by private companies. Those Managed Care Organizations (MCOs) negotiate fees with individual providers, thus, providing a greater level of accountability. Additionally, the financial risk is no longer a burden for Arkansas taxpayers, but instead is borne by the MCOs.
In short, Managed Care is about delivering access to the right care, in the right place, and at the right time.
The Diamond Care proposal, on the other hand, is an unproven piece of patchwork legislation, which does little to change the current status quo. The only change in Diamond Care is that private companies will be hired to simply administer services. Providers will continue to be paid by the state, and, therefore, taxpayers continue to assume the unpredictable financial risk.
Both plans claim to save money.
The Governor’s Managed Care plan is projected by The Stephen Group, an independent health care consultant, to save $1.4 billion. Diamond Care, on the other hand, is projected to save approximately $1 billion. The question then is this: Why leave $400 million in savings on the table?
The Managed Care plan proposed by the governor is no experimental stopgap measure or political ploy. Managed Care of Medicaid is already in effect in 40 states with great success. Diamond Care is unproven, untested and, even according to its peak projections, comes $400 million short of the savings provided to taxpayers by private Managed Care of Medicaid. With a proven track record, compelling results and a shifting of risk away from taxpayers, the future of Medicaid is clearly in Managed Care.